Diversity of Immune Response in Small-Cell Lung Cancer and Susceptibility to Immune Checkpoint Blockade
March 16, 2024
Atezolizumab (anti-PD-L1), in conjunction with carboplatin and etoposide (CE), has become established as the standard treatment for extensive-stage small-cell lung cancer (ES-SCLC). However, gaining a clearer comprehension of therapeutically significant subsets within SCLC could pave the way for rational combination strategies and ultimately enhance patient outcomes. To this end, Nabet et al. conducted comprehensive transcriptomic analyses and employed non-negative matrix factorization on 271 pre-treatment tumor samples from the IMpower133 trial. Their analysis identified four distinct subsets, which broadly align with previously reported SCLC subtypes (SCLC-A, -N, -P, and -I).
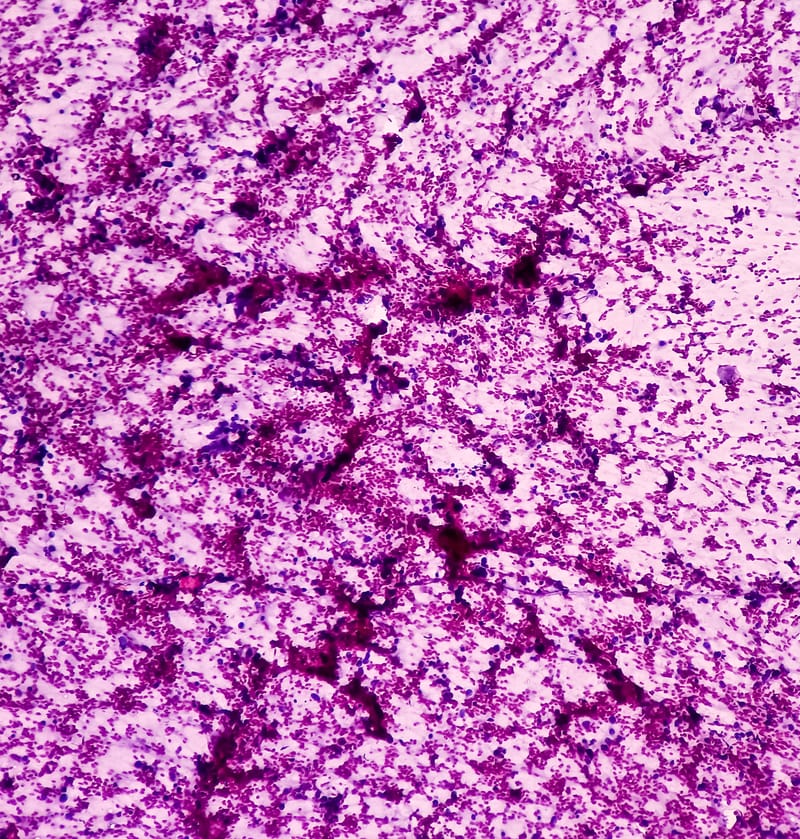
Further exploration into immune heterogeneity unveiled two subsets characterized by disparate neuroendocrine (NE) and non-neuroendocrine (non-NE) phenotypes, each exhibiting distinct immune cell infiltration patterns. Notably, NE tumors exhibiting low levels of tumor-associated macrophages (TAMs) but elevated T-effector signals demonstrated prolonged overall survival when treated with PD-L1 blockade and CE compared to CE alone, in contrast to non-NE tumors characterized by high TAM and T-effector signal levels.
This study offers a clinically relevant framework for distinguishing SCLC patients who are most likely to derive benefit from immunotherapies. Additionally, it underscores the intricate mechanisms governing responses to immunotherapy, shedding light on the complex interplay between tumor phenotypes and immune cell infiltration.
SOURCE: https://www.cell.com/cancer-cell/fulltext/S1535-6108(24)00015-1
CREDITS: CELL PRESS